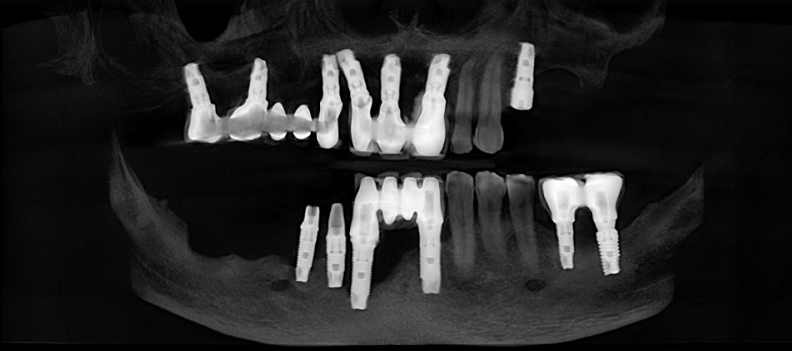
- Issues related to the implantation process (improper planning and execution, incorrect spatial positioning of the implant)
- Design of the dental restoration (difficult to clean, adhesive residue in cemented restorations, use of improper abutments, or unsuitable materials)
- Patient-related factors (smoking, uncontrolled systemic diseases such as diabetes, periodontal disease, poor oral hygiene)
- Biomechanical factors (force distribution, overload)
- Biological factors (quality of tissues, e.g., thin or mobile gums)
The surface of implants is inherently rough, as manufacturers aim to create a strong and durable connection between the bone tissue and the implant surface through various surface treatment processes. The biggest issue arises when **bacteria can adhere to and proliferate on the exposed implant surface** much more easily than on a tooth surface. As a result, the progression of the condition is faster and more aggressive than in periodontal disease.
Prevention Before Implantation:
- Existing periodontal disease (such as periodontal pockets) poses a significant risk for the development of inflammation around implants. Therefore, periodontal treatment must be performed before implantation to reduce the amount of bacteria in the mouth.
- Proper planning: If there is insufficient bone structure, bone grafting may be necessary. In cases of very thin or mobile mucosa, some form of gum correction may be required. The more tissue surrounding the implant, the better protected it is against bacteria.
Regular check-ups (every six months), professional oral hygiene treatments (scaling), and annual X-rays are essential.
In our clinic, we almost exclusively create screw-retained
zirconia implant restorations. Their greatest advantage
(besides avoiding adhesive residue around the implant) is
their removability, which allows us to periodically check
the condition of the implants and surrounding tissues more
thoroughly.
Unfortunately, many people are unaware that the subgingival part of the restoration can only be made of titanium or zirconia, with the latter providing even better gum adhesion. Unfortunately, we often see restorations where a significant amount of ceramic contacts the gum, preventing proper adhesion and increasing the likelihood of inflammation.
Unfortunately, many people are unaware that the subgingival part of the restoration can only be made of titanium or zirconia, with the latter providing even better gum adhesion. Unfortunately, we often see restorations where a significant amount of ceramic contacts the gum, preventing proper adhesion and increasing the likelihood of inflammation.
Treating peri-implantitis is very challenging, and there is currently no completely reliable treatment method. Treatments focus on cleaning the infected implant surface:
- Mechanical cleaning using special curettes and brushes
- Specialized sonic and air-polishing devices (e.g., EMS)
- Disinfection with chemical agents (e.g., chlorhexidine)