Periodontitis is one of the most insidious conditions that can occur in the human oral cavity. In some cases, there are no significant symptoms, or patients may not take them seriously (“my gums sometimes bleed”). It can develop at any age and often leads to irreversible changes. Periodontitis refers to the degradation of the tooth-supporting tissues (periodontium).
In the early stages, gingivitis develops primarily due to plaque, which is a mass of calcified bacteria. This plaque maintains a constant inflammation, which, over time, spreads to the bone beneath the gums, causing its breakdown and resorption.
Periodontitis is often asymptomatic for years, and the first symptoms may only appear when the teeth become mobile. Patients often seek treatment at this stage, but in many cases, the process is already irreversible, requiring tooth extraction due to periodontal damage.
In severe, neglected cases, periodontitis can lead to the loss of all teeth.
What causes periodontitis?
The most common cause is poor oral hygiene and increased plaque formation, although certain genetic factors and habits also play a role. For example, smoking causes vasoconstriction, reducing blood supply to the oral cavity and weakening the regenerative capacity of gum and bone tissues. Other associated conditions include those related to pregnancy and diabetes.
Fundamentally, the altered bacterial flora in the plaque on the teeth is responsible for the inflammation. If this inflammation persists, it leads to the breakdown of the tooth’s supporting structure.
What factors increase the risk of periodontitis?
Risk factors include:
- poor oral hygiene
- smoking
- diabetes
- stress
- immunodeficiency (e.g., HIV infection, post-transplantation, chronic diseases, leukemia, etc.)
- genetic factors
- hormonal changes (e.g., pregnancy)
- poor nutrition (e.g., vitamin C deficiency)
- certain medications (e.g., dry mouth as a side effect)
- local factors (e.g., non-self-cleaning or hard-to-clean areas, crowded teeth, poorly fitting fillings, crowns, or bridges)
Initially, inflammation occurs only in the superficial tissues, known as gingivitis. This condition is reversible. Therefore, regular dental check-ups are crucial for early diagnosis and treatment.
Plaque and calculus, along with the bacteria they contain, cause inflammation. This inflammation leads to swollen, red gums that may bleed upon contact.
Unfortunately, it is common for patients to avoid cleaning the affected area when bleeding occurs, or to avoid brushing altogether. This is a misconception, as proper cleaning can reduce or eliminate the inflammation and bleeding.
Soft-bristled toothbrushes are recommended, as they clean effectively without irritating the gums. Electric toothbrushes with pressure control are also advised for better plaque removal.
Flossing or interdental brushes are essential for cleaning between teeth, especially in crowded areas. Antiseptic mouthwashes like Corsodyl or Curasept are recommended to reduce inflammation.
How is periodontitis diagnosed?
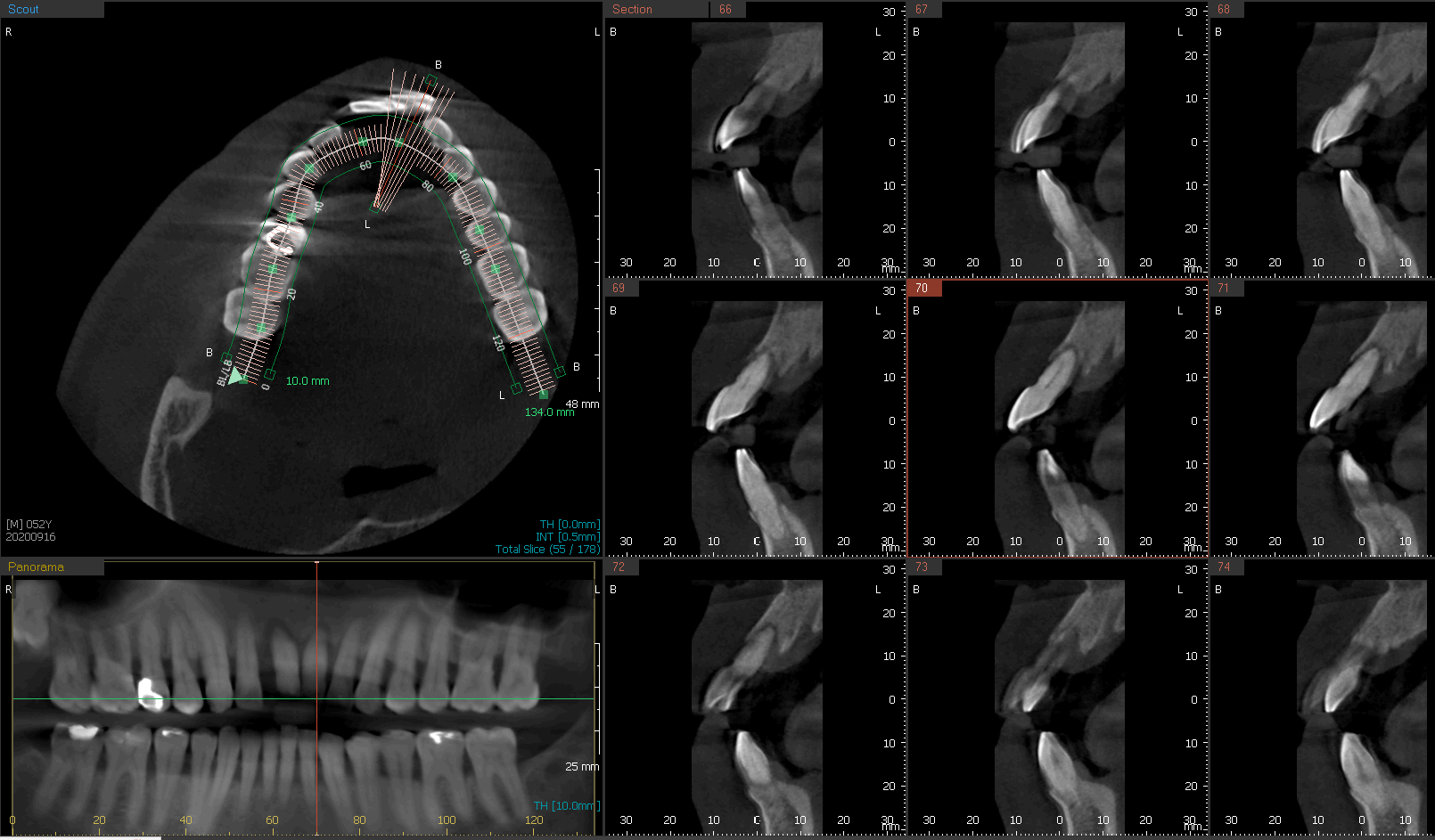
Periodontitis is diagnosed using a probe to measure pocket depths and assess bleeding. Radiographic imaging (panoramic or periapical X-rays) helps evaluate bone levels around the teeth.
What are the consequences of untreated periodontitis?
Aggressive bacteria in deep pockets cause bone loss, leading to tooth mobility and eventual tooth loss. Advanced cases may require complex treatments to restore function.
How is periodontitis treated?

Treatment involves scaling, root planing, and regular professional cleanings. Surgical interventions may be necessary for severe cases.
How can periodontitis be prevented?
- Brush teeth at least twice daily
- Use a soft-bristled toothbrush
- Consider an electric toothbrush
- Clean interdental spaces with floss or interdental brushes
- Use antiseptic mouthwash
- Quit smoking
FAQ
What are the symptoms of periodontitis?
Periodontitis is often asymptomatic, with gum bleeding or bad breath as early signs. In advanced stages, teeth may become loose.
What can untreated periodontitis cause?
Untreated periodontitis can lead to tooth loss and may require bone grafting for implant placement.
What is the treatment process?
Treatment starts with professional cleaning and hygiene education, followed by deep cleaning and possible regeneration of tooth-supporting structures.
